BJU International, Volume 83, Issue Suppl. 1, Pages 1-12. Friday, 1 January 1999.
Department of Urology, St George's Hospital NHS Trust, Tooting, London, UK
BJU International, Volume 83, Issue Suppl. 1, Pages 1-12. Friday, 1 January 1999.
Department of Urology, St George's Hospital NHS Trust, Tooting, London, UK
Despite an estimated one-sixth of the world's men having been circumcised1,2, it has long been forgotten where or why this most intriguing operation began. The procedure has been performed for religious, cultural and medical reasons, although the last has only become fashionable since the rise of modern surgery in the 19th century. Accordingly, the indications for surgery have surfaced, submerged and altered with the trends of the day. In this review we explore the origins of circumcision, and discuss the techniques and controversies that haveevolved since the event has become medicalized
.
Anthropologists do not agree on the origins of circumcision. The English egyptologist, Sir Graham Elliot Smith, suggested that it is one of the features of a heliolithic
culture which, over some 15 000 years ago, spread over much of the world. Others believe that it may have originated independently within several different cultures; certainly, many of the natives that Columbus found inhabiting the New World
were circumcised. However, it is known that circumcision had been practised in the Near East, patchily throughout tribal Africa, among the Moslem peoples of India and of south-east Asia, as well as by Australian Aborgines, for as long as we can tell. The earliest Egyptian mummies (1300 BCE) were circumcised and wall paintings in Egypt show that it was customary several thousand years earlier than that3,4.
In some African tribes, circumcision is performed at birth. In Judaic societies, the ritual is performed on the eighth day after birth, but for Moslems and many of the tribal cultures it is performed in early adult life as a rite of passage
, e.g. puberty or marriage. Why the practice evolved is not clear and many theories have been proposed. Nineteenth century historians suggested that the ritual is an ancient form of social control. They conceive that the slitting of a man's penis to cause bleeding and pain is to remind him of the power of the Church, i.e. We have control over your distinction to be a man, your pleasure and your right to reproduce
. The ritual is a warning and the timing dictates who is warned; for the new-born it is the parents who accede to the Church: We mark your son, who belongs to us, not to you
5. For the young adolescent, the warning accompanies the aggrandisement of puberty; the time when growing strength give independence, and the rebellion of youth6.
Psychologists have extended this theory to incorporate notions of pain imprinting
. By encoding violence on the brain, child-maternal bonding is interrupted and a sense of betrayal is instilled in the infant; these are considered requisite qualities that enhance the child's ability for survival later in life7. Indeed, some components of these psychological theories have recently been tested in prospective clinical trials and there is now evidence that neonates who are circumcised without local anaesthetic do have increased pain responses when 4- and 6-monthly vaccinations are administered8.
Others believe that circumcision arose as a mark of defilement or slavery1,9 (fig. 1). In ancient Egypt captured warriors were often mutilated before being condemned to the slavery. Amputation of digits and castration was common, but the morbidity was high and their resultant value as slaves was reduced. However, circumcision was just as degrading and evolved as a sufficiently humiliating compromise. Eventually, all male descendents of these slaves were circumcised. The Phoenicians, and later the Jews who were largely enslaved, adopted and ritualized circumcision. In time, circumcision was incorporated into Judaic religious practice and viewed as an outward sign of a covenant between God and man (Genesis XVI, Fig. 2).
There are many other reasons why circumcision may have evolved. Some have suggested that it is a mark of cultural identity, akin to a tattoo or a body piercing3. Alternatively, there are reasons to believe that the ritual evolved as a fertility rite4. For example, that some tribal cultures apportion seasons
for both the male and female operation, supports the view that circumcision developed as a sacrifice to the gods, an offering in exchange for a good harvest, etc. This would seem reasonable as the penis is clearly inhabited by powers that produce life. Indeed, evidence of a connection with darvests is also found in Nicaragua, where blood from the operations is mixed with maize to be eaten during the ceremony1,10. (Fig. 3). Although the true origins of circumcision will never be known, it is likely that the truth lies in part with all of the theories described.
Whatever religious or cultural forces drove this practice, historical clues to the surgical aspects of circumcision cane be found by chronicling the medical texts. However, this approach has its limitations: techniques and practitioners were diverse and studying surgical writing alone provides an incomplete reflection of the controversies that are endemic to all times. Furthermore, was it always doctors who performed the procedure in ancient times? Probably not: in biblical times it was the mother who performed the ceremony on the newborn. Gradually mohels took over; men who had the requisite surgical skill and advanced religious knowledge. After prayer, the mohel circumcised the infant and then blessed the child, a practice little changed today11 (Fig. 4a-d). In ancient Egyptian society, the procedure was performed by a priest with his thumb-nail (often gold-impregnated) and throughout mediaeval times it appears to have been largely kept in the domain of religious men12.
Few mediaeval medical texts describe the procedure, although Theodoric (1267) suggests the need for removal of the end part (penis)
in the treatment of black warts and tubercles
13. He may indeed have been describing circumcision in the context of some penile pathology. However, it is likely that doctors did not perform circumcision until the latter half of the 19thcentury.
Brief descriptions of adult circumcision for phimosis start to appear in early 19th century textbooks. Although the surgical techniques tend not to be described in detail, Abernathy (1928)14 who was a reluctant surgeon) does report the use of the bistoury (knife) to achieve circumcision in men with gonoccocal phimosis
. He also states that the bleeding should be stanched with iodoform and boric
, possibly indicating that sutures were not applied. Baillie (1833)15 also describes gonococcal phimosis and recommends that the initial treatment is nugatory
(inoperative) involving the washing of the penis (and under the prepuce with soap and tepid water, followed by the application of calomel ointment. Abernathy also warns against immediate circumcision in the face of a morbidly sensitive surface
(and declares that Sir Edward Home agrees with him!). He advocates that the posthitis (inflamed foreskin) should be allowed to soothe and allay
before surgical intervention. We can assume that the complications recognized by both Abernathy and Baillie were re-phimosis, re-stricture or suppuration; what is clear is that circumcision was not a procedure taken lightly at that time. Interestingly, neither author mentions circumcision in the neonate, suggesting that it had not yet significantly entered the domain of Englishsurgeons.
By the middle of the 19th century, anaesthesia and antisepsis were rapidly changing surgical practice. The first reported circumcision in the surgical accounts of St Bartholomew's Hospital was in 1865; although this comprised only one of the 417 operations performed that year, it was clearly becoming a more common procedure16. Indeed, this was a time when surgical cures were being explored for all ails and in 1878 Curling described circumcision as a cure for impotence in men who also had as associated phimosis17. Many other surgeons reported circumcision as being beneficial for a diverse range of sexual problems18. Walsham (1903) re-iterates the putative association of phimosis with impotence and suggests that it may also predispose to sterility, priapism, excess masturbation and even venereal disease19. Warren (1915) adds epilepsy, nocturnal enuresis, night terrors and precocious sexual unrest
to the list of dangers20, and this accepted catalogue of phimotic ills
is extended in American textbooks to include other aspects of sexual erethisms
such as homosexuality21,22.
The turn of the 19th century was also an important time in laying the foundations of surgical technique. Sir Frederick Treves (1903) provides us with a comprehensive account of basic surgical principles that remain today23. Like most of his contemporaries, he used scissors to remove the prepuce (fig. 5) and describes ligation of the frenular artery as being mandatory
in the adult. He also warns against the excess removal of skin, as this may lead to chordee.
Treves also maintains that the oppositional sutures of the skin edges must be of interrupted fine catgut
. Other surgeons chose to use horse-hair or silk19, but irrespective of variations in suturing materials, all were agreed that a continuous stitch should not be applied. One notable exception was the Master Technician and influential French Surgeon E. Doyen, who headed his own Institute of Surgical Excellence in Paris (L'Institut Doyen). Many foreign surgical trainees passed through his department, and together with his English collaborator H. Spencer-Browne, they described their antihaemorrhagic triradiate continuous circumcision suture line24. Three circular sutures of no. 1 silk were applied to achieve coaptation
of the skin edges, each one third of the circumference of the glans. The ends were not tied so as to allow expansion of the space between the two skin layers if necessary (fig. 6a). A compressing piece of sterilized muslim was then wrapped over the entire distal penis, with a snug hole to allow for the passage of the glans (Fig. 6b). The sutures and the muslin were then removed after 3-5 days.
Such variations in suture application aimed at minimizing the most frequent immediate complication of haemorrhage. Indeed, the popular urological text of Charles Chetwood (1921) recommended leaving long interrupted horse-hair sutures so that compressive strips of iodoform and petroleum gauze could be securely tied down over the suture line (Fig. 7a). Variations on what became known as chetwood's dressing
appeared as recently as Sir Alec Badenorch's Manual of Urology in 1953 (Fig 7b)25. This later text is also interesting in that measures to prevent haemorrhage within the first 24 h of surgery included the administration of stilboestrol to prevent erection of the penis. He recommended that this be given at a dose of 5 mg three times daily, beginning one day before surgery and continued for several days afterwards. He also advocated the use of bromide and chloral for similar reasons. It is also interesting that the 1974 edition of Badenoch's Manual no longer included this advice.
Neonatal circumcision techniques have evolved in parallel. It is clear from most surgical texts that circumcision of the new-born had become a regular request for the surgeon by the later part of the 19th century. For instance, Jacobsen (1893)26 warns of the importance of establishing a familial bleeding tendency from the mother before circumcision. He describes the case of four Jewish infants, each descended from a different grandchild of a common ancestress, all of whom died from haemorrhage after circumcision. Treves (1903)23 and most other contemporary writers note that ligation of the frenular arteries is usually not necessary in the neonate and that bleeding can usually be controlled by simple pressure. Indeed it seems that crush
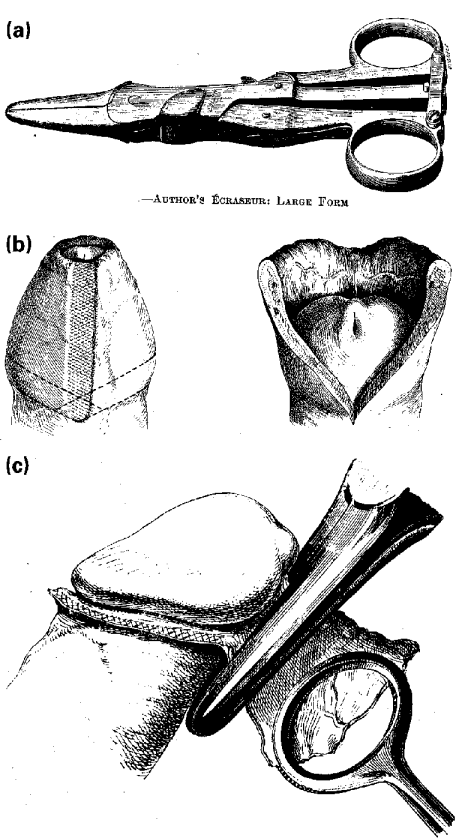
with a clamp followed by preputial excision rapidly became the template for the operation in babies. As such, the last hundred years has seen the evolution of various crushing and clamping instruments to facilitate the procedure. Doyen (1920)24 developed his Écraseur for use in neonatal circumcision. The foreskin was crushed and cut in four separate manoeuvres with very little concomitant bleeding. He was so impressed with the efficacy of this instrument that he frequently used it for adult circumcisions without (he claimed) the need for additional sutures (Fig. 8a-c).
By the 1930s, many circumcision clamps were available for use in the new-born. Indeed, the use of such clamps prompted Thomson-Walker27 to painstakingly warn of the dangers of injury to the glans when such clamps were used, and not surprisingly, more sophiticated tools were introduced to protect the penis. The prototype of the Winkelman
was introduced in 1935 and its appearance has changed little today. (Fig. 9). However, concern not only over the dangers of neonatal circumcision, but also of the risks of neonatal anaesthesia lead to the development of the Plastibell
device by the Hollister company in the 1950s (Fig. 10). Its use was first reported in 195628 and several favourable reports followed29,30. With the exception of the occasional proximal migration of the ring31,32, complications are few and the device remains in widespread popular use today. More recently plastic clamps with integral stell cutting blades have also been introduced33. These include instruments such as the GlansguardTM (Fig. 11) and many other clamps, e.g. the Gomco, Bronstein and Mogen variations, are used in different parts of the world.
Winkelmancircumcision clamp. Reproduced with permission of Aescalup Surgical Products.
More than 2000 years of Jewish persecution has led to the development of alternative surgical procedures. Indeed, uncircumcision as a measure to offset the oppression of Jews is cited in the Old Testament (I Maccabees 1:14-15) and surgical attempts to restore the prepuce have been well documented throughout history17,34,35. In modern times, this was no more true than during the period of Nazi terror, where clandestine recontructions were commonplace in a desperate attempt by Jewish men to avoid internment36. Relics of anti-Semitism are evident throughout history and even the statue of Michelangelo's David (a Jew), which was erected in Florence in 1504 was carved uncircumcised37 (Fig. 12). Not surprisingly, contemporary operations to
stretch
the circumcised foreskin are recorded in early Renaissance Europe34. In more recent surgical times, surgeons were urged to develop alternative procedures to circumcision for men who required surgery for phimosis. Cloquet's V
excision of the foreskin in 1900 was a popular means to retain a cloak
of prepuce over the glans, yet still release the phimosis38 In 1926, Young and Davies39 described a preputial-plasty whereby a constricting band of the foreskin was incised and then closed by the Heinecke-Mikulicz principle (Fig. 13). Although not widely practised, this procedure has stood the test of time and recently was shown to be superior to circumcision in a comparative study40.
Recurrent paraphimosis has long been held to be an indication for circumcision. In most circumstances, it can be reduced by manipulation, and circumcision performed electively later. However, Walsham (1903)19 recommended an alternative approach whereby acute division of the paraphimotic band was all that was necessary. He suggested that in the presence of such an oedematous prepuce, the phimotic band would heal with less constriction, and that delayed circumcision would not be required (Fig. 14). Young and Davies also described a similar procedure whereby a preputial-plasty was performed on the constricting band during the acute oedematous phase; the prepuce was reduced and the need for a circumcision negated (Fig. 15). It is interesting that a re-invention
of this operation has recently been reported41.
It is surprising that despite the many billions of foreskins that have been severed over thousands of years, it is only recently that efforts have been made to understand the prepuce. The first adequate embyrological description of preputial development was published in the 1930s42. It was realized that the formation of the preputial space occurred by patch desquamation of the epithelial cells which were contiguous between the glans and the prepuce, a process not necessarily complete by birth43. Indeed the first study to address this question was the influential landmark report of Douglas Gairdner in 194944. He concluded that only 4% of foreskins were fully retractile at birth, yet 90% were so by the age of 3 years. Of these remaining foreskins, most could be rendered retractile by gentle manipulation. Recent studies have suggested that by the age of 17 years, only 1% remain unretractile45. However, the importance of Gairdner's paper was that he was one of the first people to ascribe a function to the prepuce. Previous medical texts are notable for their absence of comment and some even describe the prepuce as a vestigial structure20,21,46. Gairdner made the astute observations that the slow period of preputial development corresponded with the age of incontinence. He felt that the prepuce had a protective role and noted that meatal ulceration only occurred in circumcised boys. Recently, a doctor writing anonymously in the BMJ provided an analogy suggesting that the prepuce is to the glans what the eyelid is to the eye47.
To date, a more definite function cannot be ascribed to the prepuce, but as an accessible and ready source of fibroblasts, it has become a favourite tissue reservoir for cell-culture biologists and hence basic scientific research. From this wealth of disparate information, it is clear that the foreskin is an androgen-dependent structure48 with complex intradermal enzyme systems. These confer upon it a wide range of metabolic functions, including the differential metabolism of various prostaglandins which are copiously produced throughout the male and female genital tract49. Certainly, it can be anticipated that many other biochemical functions will be defined in the years to come; a vestigal structure it almost certainly is not40.
Notwithstanding the relative disinterest over the function of the prepuce, no other operation has been surrounded by controversy so much as circumcision. Should it be done, then when, why, how and by whom? Religious and cultural influences are pervasive, parental confusion is widespread and medical indications shift with the trends of the day. Doctors divide into camps driven by self-interest, self-righteousness and self-defence. It is not surprising that some of the most colourful pages in the medical literature are devoted to the debate. For instance in 1950, Sir James Spence of Newcastle upon Tyne responded to the request from a local GP as follows:
…Your patient C.D., aetat 7 months, has the prepuce with which he was born. You ask me with a note of persuasion in your voice, if it should be excised. Am I to make a decision on scientific grounds, or am I to acquiesce in a rate which took its origin at the behest of that arch-sanitarian Moses?…If you can show good reason why a ritual designed to ease the penalties of concupiscence amidst the sand and flies of the Syrian deserts should be continued in this England, land of clean bed-linen and lesser opportunity, I shall listen to your arguments ……(do you not) understand that Nature does not intend it (the foreskin) to be stretched and retracted in the Temples of the Welfare Centres or ritually removed in the precincts of the operating theatres…51.
Literary assaults such as these have served to fuel the debates and even a Medline® search today reveals that in the last year alone, 155 reviews or letters have been published arguing for or against routine circumcision. However, studying the evolution of the medical indications provides us with a pleasing demonstration of how controversy drives scientific enquiry. We have already described how the surgeons of 100 years ago advocated circumcision for a wide variety of conditions, such as impotence, nocturnal enuresis, sterility, excess masturbation, night terrors, epilepsy, etc. There can be no doubt that a large element of surgical self-interest drove these claims. However, most of the contemporary textbooks also included epithelioma (carcinoma) of the penis amidst the morass of complications of phimosis. Although rare, once this observation had been made, it presumably filtered down through the textbooks by rote, rather than scientific study. A few reports had appeared in the early 20th century indicating that carcinoma of the penis was rare in circumcised men, but not until the debate over neonatal circumcision erupted in the medical press in the 1930s that this surgical mantra
was put to the test. In 1932, the editor of the Lancet challenged Abraham Wolbarst52, a New York urologist, to prove his contention (in a previous Lancet editorial), that circumcision prevented penile carcinoma. Wolbarst responded by surveying every skin, cancer and Jewish hospital in the USA, along with 1250 of the largest general hospitals throughout the Union. With this survey, he was able to show that penile cancer virtually never occurred in circumcised men and that the risk related to the timing of the circumcision. Over the years this association has been reaffirmed by many research workers, although general hygiene, demographic and other factors such as human papilloma virus and smoking status are probably just as important53. However, Wolbarst established that association through formal scientific enquiry and proponents of the procedure continue to use thisas a compelling argument for circumcision at birth.
Almost as an extension to the lack of penile cancer in Jews, Handley54 reported on the infrequency of carcinoma of the cervix in Jewish women. He suggested that this related to the fact that Jewish men were circumcised. Not surprisingly, this spawned a mass of contradictory studies and over the next 50 years the champions of both camps have sought to establish the importance or irrelevance of circumcision in relation to penile cancer. The pendulum has swung both ways and the current evidence suggests that other factors are probably more important55,56. A similar debate has raged for 50 years over concerns for the risks of urinary tract infections in young boys and currently, any decreased risk associated with circumcision remains tentative but notproven56.
However, during the two World Wars, governments became increasingly interested in reducing the risk of venereal disease amongst their soldiers. Clearly, such pathology can have a profound effect on the efficiency of fighting armis. Indeed, in 1947 the Canadian Army57 found that whereas 52% of their soldiers had foreskins intact, 77% of those treated for venereal disease were uncircumcised. Persuasive arguments to circumcise all conscripts were proposed. Furthermore, it was an age-old observation, and indigenous African healers had promoted circumcision to prevent the transmission of sexually transmitted disease for centuries58. As might be expected, the evidence did not withstand further scientific scrutiny and numerous contradictions were provided56 However, there has recently been startling evidence that HIV infection is significantly associated with the uncircumcised status59. Indeed, one author has recently suggested routine neonatal circumcision on a world-wide scale as a long-term strategy for the control of AIDS60: a whole new chapter opens in this ancient debate!
Finally, controversy has arisen over who should perform the procedure. Once circumcision had been medicalized
in the 19th century, many surgeons were keen to take paying customers away from the religious men. As such, doctors were often quick to highlight the unforseen risks attendant on a non-medical procedure. For instance, Cabot (1924)61 described tuberculosis of the penis occurring when Rabbis with infected sputum sucked on the baby's penis to stop the bleeding. However, it has often been claimed that the incidence of complications in Jewish children is very low and that the final result is usually better than any hospital doctor can produce62,63. Naturally, quality control is variable and whereas not all commentators have had such respect for the religious men64,65, others have been quick to indicate the sub-optimal results frequently obtained in hospital29. Not surprisingly, disastrous accounts damning practitioners from all quarters have embellished the literature on countless occasions. Irrespective, the circumcision of young boys has become a thriving business for all parties66.
However, with a healthcare budget of $140 million per year in the USA (1990)67, insurance companies eventually forced closer scrutiny. Following such pressure, the first Task Force of Neonatal Circumcision from the American Academy of Pediatrics (1n 1975) concluded that there was no valid medical indication for this procedure68. However, the pro-circumcision lobby was strong and the task force was forced to re-evaluate. In 1989, they conceded that there may be certain advantages to neonatal circumcision, although their recommendations did stop short of advising routine operation56. Similar pressures in the UK have now resulted in only certain Health Authorities being prepared to pay for the procedure. These tend to be in regions with large ethnic minorities who otherwise may suffer form back street
circumcisions62,64.
Thus it is clear that medical trends are now being driven by financial constraints. Perhaps this is reflected by the dramatic decline in the number of non-religious circumcisions performed over the last half century; in the USA an estimated 80% of boys were circumcised in 197669 but by 1981 this had fallew to 61%67, and recent estimates suggest that this decrease continues70. In the UK the decline has been even more dramatic: originally more common in the upper classes44, circumcision rates fell from 30% in 1939 to 20% in 1949 and 10% by 1963. By 1975 only 6% of British schoolboys were circumcised71 and this may well have declined further63. Whether this general trend reflects a tempering of attitudes towards the persuasive medical rhetoric that has simmered for the past 100 years, or whether financial considerations have dampened enthusiasm, is unknown. Perhaps the First World cultures are witnessing an escape from the medical paternalism that has gripped them for so long, or even that the age-old ritual is simply no longer fashionable in modern peoples; again, it is unknown. However, whatever the current trend, ebbing or flowing, we can be sure that the controversies of circumcision will continue to colour the medical literature, far into the future.
Many historical accounts of circumcision have been written and most authors have used their survey to form an opinion as to whether the neonatal procedure is justified. The weak medical arguments are tempered by the importance of cultural and religious factors. In truth, the real reasons why circumcision has evolved are much broader. Opponents of the ritual draw attention to the rights
of the new-born, which, they argue, mut be upheld66. Others contest that humans are social animals and cannot survive alone; they require their parents, community and culture to thrive, and, as such, rights
belong to the group, not to the individual. If there is an inherent survival advantage to a group of humans who chose to maim their young, then this is presumably evidenced by their continued survival as a race11. In short, to conclude any historical reflection with a reasoned right
or wrong
, would be like claiming to have fathomed human nature itself. Consider this; mankind has developed this strange surgical signature that is so pervasive, that in the last five minutes alone, another 120 boys throughout the world have been circumcised.
Davidof Michelangelo or
why the foreskin?. JAMA 1971; 218: 1304
W.D. Dunsmuir, Specialist Registrar, South-west Thames Region
E. M. Gordon, Consultant Urologist.
Correspondence: Mr Dunsmuir, Department of Urology, St George's Hospital NHS Trust, Blackshaw Road, Tooting, London SW17 OQT, UK
The Circumcision Information and Resource Pages are a not-for-profit educational resource and library. IntactiWiki hosts this website but is not responsible for the content of this site. CIRP makes documents available without charge, for informational purposes only. The contents of this site are not intended to replace the professional medical or legal advice of a licensed practitioner.
© CIRP.org 1996-2025 | Filetree | Please visit our sponsor and host:
IntactiWiki.